Short CommentaryOpen Access, Volume 2 Issue 3
Initial Simple Questionnaire for Premorbid Global Function in Acute Stroke Patients
Anusha Gadipudi1*; Maya Muhanna1 ; Austin Helton1 ; Nisha Kashyap1 ; Sunil Mathur2 ; Fenwick T Nichols3 ; Askiel Bruno3
1Medical College of Georgia, USA.
2Houston Methodist Research Institute and Houston Methodist Neal Cancer Center, Houston, Texas, USA.
3Department of Neurology, Medical College of Georgia, Augusta University, USA.
*Corresponding author: Askiel Bruno
Department of Neurology, Medical College of Georgia, 1120 15th Street, BI 3076, Augusta, GA 30912, USA.
Email: bruno@augusta.edu
Received : Apr 05, 2024 Accepted : May 16, 2024 Published : May 23, 2024
Epidemiology & Public Health - www.jpublichealth.org
Copyright: Gadipudi A © All rights are reserved
Citation: Gadipudi A, Muhanna M, Helton A, Kashyap N, Mathur S, et al. Initial Simple Questionnaire for Premorbid Global Function in Acute Stroke Patients. Epidemiol Public Health. 2024; 2(3): 1052.
Abstract
Background: Knowing a patient’s premorbid functional status can aid in acute stroke management decisions. The often-adopted modified Rankin Scale is not suitable for prestroke assessment as it lacks a defined comparison state at lower scores.
Methods: We designed a simple questionnaire for prestroke functional status assessment and tested its clinimetric properties in acute stroke patients. Five investigators took part in scoring the novel scale. For reliability testing, two raters independently administered the novel scale on two consecutive days to the patients or their caregivers, or both. For validity testing, one rater administered the Groningen activities scale and the other rater administered the Lawton activities scale on the two consecutive test days.
Results: We tested 50 patients within 3 days of admission. The reliability kappa statistic between the paired raters was 0.36, and the weighted kappa (accounting for the degree of disagreements) was 0.53. Validity of the novel scale against the two validated function scales was moderate (correlation coefficients 0.65 and -0.56).
Conclusion: We believe that misunderstandings of the novel questions by interviewees likely lead to weak reliability. These novel results inform the design of future research on this topic with clarified simple and unambiguous questions.
Keywords: Functional status; Ischemic stroke; Hemorrhagic stroke, Independence.
Introduction
Rapid and accurate estimation of premorbid functional status in patients presenting with acute stroke is often desired for outcome estimation and qualification for acute stroke treatment trials. The often-adopted modified Rankin Scale (mRS) [1] is not suitable for premorbid assessment of independently functioning people, because prior to stroke there is no defined comparison state needed to differentiate between scores 0, 1, and 2 [2].
Some of the currently validated baseline function scales assess primarily basic activities of daily living, some assess primarily instrumental activities, and some were designed for estimating cognitive impairments [3]. Ideally, a simple, accurate, and reliable tool to assess baseline global function among independent people, analogous to the mRS, could help make management decisions during acute stroke. Therefore, we developed and tested a novel simple questionnaire to estimate a baseline (premorbid) global function.
Methods
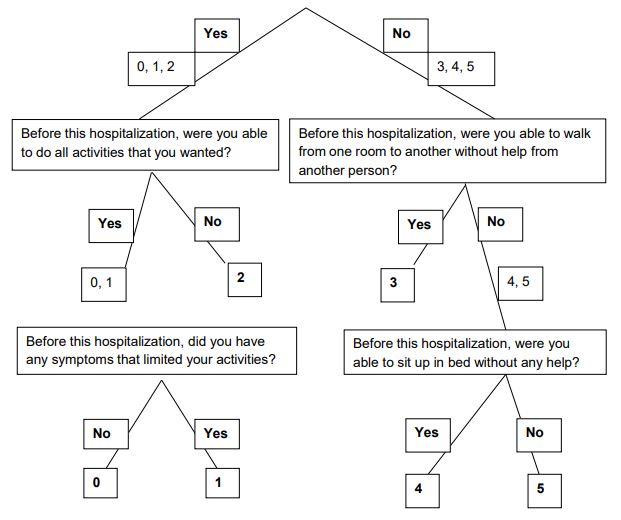
Our novel global functional status questionnaire (Figure 1) was modeled on the validated simplified mRS questionnaire (smRSq) [4]. The first question about dependent living and the two questions regarding dependent status (mRS scores 3-5) are the same as in the smRSq. Two novel questions were created to score baseline global functional status as 0, 1, or 2 among patients who declared ability to live independently prior to their stroke (left side of questionnaire, Figure 1).
All confirmed acute stroke patients, ischemic stroke or intracerebral hemorrhagic, admitted to our hospital were considered eligible if the study could be completed within 3 days after admission. Five investigators performed all the ratings. Caregivers were interviewed together with patients when they were available or when patients were unable to participate. Patients unable to participate and without an available caregiver were excluded.
For reliability testing of the novel questionnaire, patients were interviewed on two consecutive days by different raters. The order of the raters was based on the availability of the raters. We also administered two validated function scales (Groningen and Lawton) [5,6] to assess the validity of the novel scale. One of these scales was administered on the first interview day and the other on the second day.
At the conclusion of each interview, all scores were final. The raters on the second day were blinded to the scores from the first day. We avoided providing clarifications for the questions to minimize rater bias.
The kappa statistic measured the agreements between the two raters of the novel scale. The Pearson correlation statistic compared the novel scale to the two previously validated baseline function scales.
Results
Fifty patients completed all questionnaires and were included in this analysis. The mean age was 64 (SD 13) years, 46% were men, 50% were White race, 42% were Black race, and 8% were other or unspecified race. Comparing the novel scale to the Groningen scale the correlation coefficient was 0.65 (p<0.001) and comparing it to the Lawton scale the coefficient was -0.56 (p<0.001). Table 1 shows the inter-rater agreements of the novel scale with the kappa statistic of 0.36 and the weighted kappa of 0.53.
Discussion
The initial question of the smRSq has previously been shown to reliably distinguish between premorbid functional independence and being dependent on others (agreement between raters 94-96%) [4]. The two novel questions in this study were intended to more precisely identify the level of functional independence as 0, 1, or 2.
Although the novel scale shows moderate validity, the low interrater reliability currently limits its usefulness in clinical practice or research. Based on our experience with this scale, we suspect that the low interrater reliability can be partly accounted for by diverse interpretations of the two novel questions by the subjects on the two interview days. In addition, some subjects may have mistakenly responded in reference to different time points on the two interview days; their poststroke state versus the intended pre-stroke state. This likely accounts for the widely divergent scores by two investigators of 0 and 3 in two subjects (Table 1). Enhanced investigator training to better inform the subjects about the intent of this questionnaire will likely improve the accuracy of the answers.
Despite the limited usefulness of the novel questions used in this study, our findings could optimize the design of future similar questionnairs. We believe that further research in this direction, with clarified, simple, more objective questions, and more intensive investigator training in scale administration is warranted.
Patient ID: _______________
Date: _______________
Rater ID: _______________
Before this hospitalization, were you able to live alone without any help from another person? This means being able to bathe, use the toilet, shop, prepare or get meals, and manage finances.
Table 1: Agreements of scores between raters on the novel questionnaire.
| Second rater scores | |||||||
|---|---|---|---|---|---|---|---|
| First rater scores | 0 | 1 | 2 | 3 | 4 | 5 | Total |
| 0 | 25 | 3 | 0 | 0 | 0 | 0 | 28 |
| 1 | 6 | 4 | 2 | 0 | 0 | 0 | 12 |
| 2 | 1 | 2 | 0 | 0 | 0 | 0 | 3 |
| 3 | 2 | 0 | 1 | 3 | 0 | 0 | 6 |
| 4 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 34 | 9 | 3 | 4 | 0 | 0 | 50 |
References
- van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988; 19(5): 604-7. http: //www.ncbi.nlm.nih.gov/pubmed/3363593
- Bruno A, Switzer JA, Durkalski VL, Nichols FT. Is a prestroke modified Rankin Scale sensible? Int J Stroke. 2011; 6(5).
- Mlinac ME, Feng MC. Assessment of Activities of Daily Living, Self-Care, and Independence. Arch Clin Neuropsychol. 2016; 31(6): 506-16. https: //academic.oup.com/acn/article-lookup/doi/10.1093/arclin/acw049
- Bruno A, Akinwuntan AE, Lin C, Close B, Davis K, et al. Simplified modified rankin scale questionnaire: Reproducibility over the telephone and validation with quality of life. Stroke. 2011; 42(8): 2276-9.
- The Groningen Activity Restriction Scale for measuring disability: its utility in international comparisons. 2023. https: //ajph.aphapublications.org/doi/epdf/10.2105/AJPH.84.8.1270
- Lawton MP, Brody EM. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. The gerontologist. 1969; 9(3): 179-86.