Research ArticleOpen Access, Volume 2 Issue 2
Trends in Incidences, Prevalence Cases, and the Disability-Adjusted Life-Years of Bipolar Disorder in China, 1990-2019
Qiong-Qiong Zhong1,2†; Hui Zuo1†; Jun-Xiao Li1,2; Feng1*
1Department of Prevention and Health, Central Laboratory, Guangzhou Twelfth People’s Hospital, China.
2Department of Public Health and Preventive Medicine, School of Medicine, Jinan University, No.601 West Huangpu Rd., Guangzhou 510620, China.
†Joint first authors.
*Corresponding author: Feng Zhu
Guangzhou Twelfth People’s Hospital, No.1 Tianqiang St., West Huangpu Rd., Guangzhou 510620, China.
Received : Mar 20, 2024 Accepted : Apr 11, 2024 Published : Apr 18, 2024
Epidemiology & Public Health - www.jpublichealth.org
Copyright: Zhu F © All rights are reserved
Citation: Zhong QQ, Zuo H, Li JX, Zhu F. Trends in Incidences, Prevalence Cases, and the Disability-Adjusted Life-Years of Bipolar Disorder in China, 1990-2019. Epidemiol Public Health. 2024; 2(2): 1041.
Abstract
Objectives: Studies on Chinese bipolar disorders are incomplete and lagged to date.
Methods: We used the join point regression program to assess the incidence, prevalence, and disease burdens of Chinese bipolar disorders, based on the Global Burden of Disease exchange database.
Results: We observed the increasing trends in the incidence and prevalence of Chinese bipolar disorder in 1990- 2019, with increases of 22.26% in incidence number, 40.73% in prevalence number, and 17.12% in prevalence rate; wherein females had a higher prevalence rate in 1990-2019 and a higher incidence rate in 1990-2013 but a reversed trend thereafter; the Disability-Adjusted Life Years (DALY) increased by 78% for number and 15.81% for rate, respectively; those aged 30-34 shared the highest DALY number in 2019 (73,194; 95% UI (Uncertainty Interval): 43,128-113,623); the DALY-related Annual Percentage Change (APC) in 1990-2019 was 1.21% (P=0.000).
Conclusion: Bipolar disorder is being developed into an immense societal burden in China. An essential intervention strategy should be formulated earlier to better identify and treat bipolar disorders so that we can reduce negative outcomes and DALY in China.
Keywords: Bipolar disorder; Disease burden; Disability-adjusted life-years.
Introduction
Bipolar disorder is a severe psychological disorder with both manic and depressive episodes at normal intervals. Manic episodes manifest in high spirits or irritable moods, hyperactivities, rapid speeches, inflated self-esteem, and decreased sleep needs; those with manic but without depressive episodes are also classified as bipolar disorders [1]. Among bipolar disorder’s subtypes, type I manifests manic episodes, and patients are commonly in abnormal moods and worsened persistently as lengthier (≥7 days) and severer episodes (or those requiring hospitalization) with or without psychotic features; type II manifests at least a depressive episode or manic episode with briefer (≥4 days), and a moderate episode of irritable moods [2]. These subtypes rest essentially on the severity of irritable moods, although bipolar disorders do feature Major Depressive Episodes (MDD), nor are hypomania only found in Type II, and the severity of symptoms for the mixed states is not sufficient to meet the complete criteria for any of the aforementioned mental disorders.
Patients with bipolar disorder had more obstacles to work and increased unemployment due the strained family relationships [3,4]; the advanced patients were vulnerable to an impairment of working ability in males [5], which indicates that sex perspective in bipolar disorder needs to be focused. More than half of the related caregivers had experienced moderate burdens on psychological support, practical assistance, and housekeeping in the older populations with bipolar disorder [6], which suggests that the age perspective in bipolar disorder needs to be evaluated. In China, patients with bipolar disorder were susceptible to higher levels of the Body Mass Index and plasma homocysteine [7]; therefore, bipolar disorder should be a risk factor for cardiovascular diseases that are the leading cause of death in China in the past decade [8].
Globally, the prevalence of bipolar disorders, which was ranked 17th among all causes of health loss in 2013 [9], varied slightly across regions [10]; its patients reached 4.53 million in 2017, with an increase of 47.74% for the number of incidence cases from 1990 to 2017, wherein India, China, and Brazil filed the largest number of incidence cases in 1990 and 2017, and the South Asia shared the greatest numbers of incidence cases and the Disability-Adjusted Life-Years (DALYs) in 2017 [11]. There were large variations in the prevalence figures of bipolar disorder across studies. For example, the 12-month prevalence the lifetime and 1-year prevalence of bipolar disorder type 1 and type 2 in the USA adults was 1.7% in a systematic review and meta-analysis of (Kessler et al., 2012), 0.17%-0.50% in China 12-14, and 0.84% among 25 population- or community-based studies and 276,221 participants in MEDLINE, Scopus, Web of Science, PsycINFO, and the reference lists of identified studies (Clemente et al., 2015).
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) provides an opportunity to incorporate newly available datasets, enhance method performance and standardization, and respond to outbreaks of scientific knowledge. Due to various premature deaths and disabilities caused by human diseases, a series of scientific assessments for the burdens of disease’s progress and adverse patterns need to be conducted. Here, we assessed systematically the burdens of Chinese bipolar disorders including incidence, prevalence, and these indicators by age and sex, to provide a foundation for prevention and treatment, and clinical decision-making in bipolar disorder.
Methods
Data source
All study data were taken from the GBD 2019, a publicly available resource online “http://ghdx.healthdata.org/gbdresults-tool” by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, the World Health Organization (WHO), and the members of the Global GBD Collaborative Group. The GBD 2019 is an ongoing effort, updated annually, and allows for consistent comparison over time from 1990 to 2019, by age and sex, and across locations. It also produces standard epidemiological and summary measures and can be estimated from life tables, estimates of prevalence, and disability weights. The GBD study complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) guidelines for reporting health estimates As described in a previous study [15], we made a range of selections by taking region, disease cause, and indicators such as “China”, “B.6.3 bipolar disorder”, “incidence”, “prevalence” and “DALY”, respectively.
Mental disorders classification and indicator interpretation
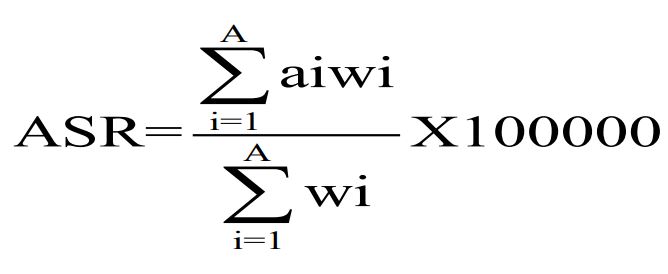
Each cause and related state covers the years 1990 to 2019 and was identified with standard case definitions. Mental disorders classification was conducted according to the International Statistical Classification of Diseases and the Related Health Problems Ninth Edition (ICD-9) and the Tenth Edition (ICD-10). Bipolar disorder was identified as the codes in the International Statistical Classification of Diseases and the Related Health Problems Ninth Edition (ICD-9) (296-296.16, 296.4-296.81) and the Tenth Edition (ICD-10) (F30-F31.9, F34.0) [16]. Due to the lack of deaths and the Years of Life Lost (YLL), we focused mainly on incidence, prevalence, and age-standardized indicators (age-standardized incidence rate and age-standardized prevalence rate). Bipolar disorder burden was mainly described with DALY, which reflects health hazards linked to disability, death, and weight on age and loss of time. The Age Standardized Rate (ASR) was calculated with a non-weighted mean of the GBD year’s age-specific proportional distributions for national locations with populations of more than 5 million in the GBD year to update the world population age standard [15]. In brief, ASR was generated from several parameters, including a summingup age-standardized rate (ai , wherein i is the ith age class), a number (or the weight) of persons (wi ) in the same age subgroup i (a reference of the standard population), and a dividend of summing-up standard population weights: [11].
Measurement and diagnosis
Study methods were described in detail on an official website (http://www.healthdata.org/gbd/). To allow the comparability in measurements, case identification adhered predominantly to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) or the ICD-10 criteria, since they were used by the majority of mental health surveys included. Bipolar disorders were included in the GBD 2019, and their identifications were a combined estimate of all subtypes. Trends in the prevalence and incidence of bipolar disorders were calculated in this study.
Data analysis
Point prevalence and point incidence were assessed in this study. A total of 14 groups, including 10-14, 15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65-69, 70-74, 75-79, and ≥80, were given due to the missing of the patients aged <10, with a start from those aged 10 years and the dividends by 5 years; the analyses by sex and age were also conducted. All data were organized and visualized with Excel 2010 and were analyzed with the Join Point Regression Program software (4.9.0.0) (https://surveillance.cancer.gov/joinpoint/). As one way to characterize trends in the rates in all of the times, the Annual Percent Change (APC) was conducted to describe temporal trends for disease burdens by an equation: ln(y) = x×b, wherein time series were built and taken as independent variables (x) and age-standardized incidence rate and age-standardized prevalence rate were taken as dependent variables (y). Horizontal and vertical comparisons to trends of disease burdens were commonly used in the indexes over a long-term interval according to public health research [17]. Statistical significance was defined as P<0.05 (two-sided). All values for each metric were represented as UIs using the 25th and the 975th ordered 1000 draw values of posterior distributions [15].
Results
Overall incidence and prevalence
The numbers of incidence and prevalence of Chinese bipolar disorders showed increasing trends in 1990-2019, with an increase of 22.26% and an increase of 40.73%, respectively; the incidence numbers had an increasing trend in 1990-2005 but a slow decline thereafter; the prevalence rates increased by 17.12%, from 1990 (183.90 per 100,000 (95% UI: 154.48-216.18 per 100,000)) to 2019 (215.38 per 100,000 (95% UI: 184.46- 249.87 per 100,000)). No significant changes in the incidence and prevalence rates-related ASRs were observed (Table 1).
Incidence and prevalence by sex and age
The incidence of Chinese bipolar disorders considerably fluctuated by sex from 1990 to 2019, with a higher incidence for females from 1990 to 2013 but for males thereafter; on the other hand, the prevalence by sex slightly fluctuated, with a slow increment and a higher level for females. Nevertheless, no significant increases in the incidence- and prevalence-related ASR were observed (Figure 1).
The incidence of Chinese bipolar disorders fluctuated across all age groups, with insignificant trends in 1990 and 2019. Those aged 15-19 shared the highest incidence, with 34.55 per 100,000 (95% UI: 24.29-45.56) in 1990 and 34.87 per 100,000 (95% UI: 24.64-46.07) in 2019, respectively; those aged 10-14 shared the lowest prevalence in 1990 (51.67 per 100,000 (95% UI: 33.61-74.61)) and in 2019 (52.72 per 100,000 (95% UI: 34.35-76.41)), respectively (Figure 2).
Bipolar disorders burdened by sex and age
The DALY numbers of Chinese bipolar disorders showed an increasing trend, with an increase of 78% from 1990 (476,231 (95% UI: 291,157-731,334)) to 2019 (662,635 (95% UI: 405,797- 1,014,648)); the DALY rates increased by 15.81% from 1990 (40.23 per 100,000 (95% UI: 24.59-61.78)) to 2019 (46.59 per 100,000 (95% UI: 28.53-71.34)). In contrast, no significant change in the DALY rate-related ASR was observed (Table 2).
Numbers and rates of DALYs showed increasing trends in males and females in 1990-2019. For DALY numbers, males had an increase of 38.11% from 1990 (235,144 (95% UI: 143,122- 364,619)) to 2019 (324,767 (95% UI: 200,080-496,791)); females had an increase of 40.14% from 1990 (241,087 (95% UI: 147,476-366,747)) to 2019 (337,867 (95% UI: 207,339- 517,165)). For DALY rates, males had an increase of 16.27% from 1990 (38.53 (95% UI: 23.45-59.75)) to 2019 (44.80 (95% UI: 27.6-68.54)); females had an increase of 15.25% from 1990 (42.03 (95% UI: 25.71-63.95)) to 2019 (48.44 (95% UI: 29.72- 74.14)). Whatever the DALY number or the DALY rate, a higher level was shared by females; additionally, no significant change in the DALY rate-related ASR was observed in 1990 and 2019 (Table 2).
Table 3 shows that the peaks of DALY numbers were shared by those aged 20-24 in 1990 (73,594 (95% UI: 41,207-116,895)) and those aged 30-34 in 2019 (73,194 (95% UI: 43,128- 113,623)), respectively.
Trends in indicators of bipolar disorders burden
Table 4 shows that the incidence- and prevalence-related APCs in 1990-2019 were 0.17% (P=0.002) and 0.66% (P=0.000), respectively; the incidence- and prevalence-related APCs of age-standardized rates in 1990-2019 were -0.0096% (P=0.035) and 0.0035% (P=0.053), respectively; the DALY-related APC in 1990-2019 was 1.21% (95% CI: 1.12-1.30, P=0.000).
Discussion
In this study, we based on the Global Burden of Disease Database to assess a series of indicators of burdens on bipolar disorders including incidence, prevalence, and DALY. We found that the numbers of incidence and prevalence of Chinese bipolar disorders increased over the past three decades, which seems to link a large population and a slow growth rate. A total of 1.41 billion populations were taken from the seventh census in 2020, with 72.05 million more than the last in China [18]; meanwhile, the increment of examination and diagnosis has been led for bipolar disorders due to dissemination and public awareness of psychological disorders and an improvement in medical technologies for past three decades since the issuing and taking effect of the Mental Health Law of the People’s Republic of China (May 2013) and the Guiding Opinions on Strengthening Mental Health Services (January 2017).
We showed a considerably fluctuating pattern of incidence by sex of Chinese bipolar disorders in 1990-2019, there are some notable for females with a higher incidence level in 1990- 2013 but males thereafter. A slight increment pattern of prevalence by sex especially in males and females was noted, females also shared more DALY cases but more rapid growth in males in recent years in this study, which is not similar to a previous report wherein the 12-month prevalence was higher in females (0.19% (0.11-0.33)) than males (0.10% (0.05-0.24)) [12,13] except for higher prevalence in males (0.22% (0.13-0.31)) but females (0.17% (0.09-0.25)) [12,13] and no significance (P=0.622) in males (0.5% (0.3-0.7)) and females (0.4% (0.3-0.6)) [14]. Although there is a contradiction when sex is taken into account, it seems highly likely that variations in bipolar incidence by sex may well be primarily attributed to awareness and societal changes [10].
A pattern of differential incidence by age was observed including insignificant trends, the highest incidence for those aged 15-19, and the lowest prevalence for those aged 10-14 in 1990 and 2019. Like a report in Australia [19], our results also reveal that DALY was centralized mainly in those aged 20-34 and females aged 15-35 were more susceptible to bipolar disorder, which hints that adolescents especially females are unstable populations who are in a complex psychological health state, careless of the knowledge of mental disorders, and experience hormone changes (especially thyroid hormone) or sensitivities [19]. Additionally, adolescent patients with bipolar disorder are still difficult to diagnose in time or successfully treat [20].
Previous literature reveals that the burden of bipolar disorders was linked to genetic factors, dietary habits, childhood and adolescent anxieties, behavioural disorders, and a family system and functioning [21-24]. As an easy relapse, bipolar disorder is related to not only main clinical features and cognitive dysfunctions but also poor outcomes, more co-morbidities, and suicide. On the societal side, bipolar disorder generates directly or indirectly a lot of costs, which therefore significantly impacts the related caregivers [3]. Taking the increasing prevalence and incidence and the updated diagnostic criteria in time into consideration, positive feedback from national policy in China appears to have emerged in recent years. The China Brain Initiative, which launched in 2016, focuses on three neurologic and neuropsychiatric diseases: autism in children, depression in adults, and Alzheimer’s Disease (AD) in the aged population [25]; naturally, the related attention specific to the prevention and treatment of bipolar disorders in China has been paid since then. We release a worsening burden on bipolar disorders from 1990 to 2019 in China, especially younger populations, which suggests that more patients with bipolar disorder have been detected and the awareness of mental disorders has increased in recent years; furthermore, adequate attention should still be paid to those aged 15-34, especially females, with bipolar disorder as soon as possible, and early interventions should be proposed as a positive strategy to better identify and treat and reduce the negative burden on society. Additionally, bipolar disorders have a high risk of relapse, which continuously impacts patients throughout their adult lifetime and contributes to a high DALY level by those aged 20-34 [11]. Thus, community administrators should play crucial and critical roles in dealing with primary care in their communities.
Implications and limitations
The ethnological mechanism of bipolar disorder has not been elucidated, although suicide has held the highest in all psychiatric disorders, with 20-30 times the general population [26]. Nevertheless, no special treatments besides medications, psychological interventions, and care or support are available for bipolar disorder. Taking significant impacts on patients, caregivers, and society into account, an urgent task for interventional strategies needs to be implemented earlier among populations with bipolar disorder at early stages [3].
There are limitations to this study. First, some information (including death number and mortality rate) was unavailable in the GBD database, and an incomplete data led our analyses only on incidence, prevalence, and DALY. Second, we cannot conduct regional surveillance and epidemiological investigations for Chinese bipolar disorder because database covers incomplete regional information. We will do further research in regional surveillance and epidemiological investigations in the future, such as using uniform assessment methods to evaluate subtypes of bipolar disorders, so that be convenient for researchers to compare and analyze, administrators to make efficient policies, and clinicians to precisely intervene or successfully treat. Nevertheless, we did our best to assess the disease burden on current bipolar disorders. It is believed that an important reference should be provided for the reconfiguration and decision-making of national healthcare resources in China.
Conclusion
Bipolar disorder has led to a large number of cases in the past three decades, wherein the youngsters are mainly centralized; an essential intervention strategy should be formulated earlier to better identify and treat bipolar disorders so that we can reduce negative outcomes and DALYs in China.
Declarations
Funding: This work was supported by the Guangzhou Municipal Science and Technology Project (201704030132, 2024A03J00721) and the Guangdong Medical Research Foundation (A2022209). The funders had no role in the design, data collection analysis, or preparation of the manuscript.
Ethics and consent: No requirement of an informed consent statement for publication because study data included in this study were de-identified and publicly available from the Global Burden of Disease (GBD) Data Exchange database.
Conflicts of interest: Authors report there are no competing interests to declare.
Acknowledgments: We appreciate the works of the Global Burden of Disease study 2019 collaborators.
Author’ contributions: ZQQ and LJX made contributions to the acquisition, interpretation, and analysis of data and Writing -the original draft; ZH made contributions to the conceptualization and content review; ZF made contributions to conceptualization, Writing - review & editing. All authors have read and agreed to the published version of the manuscript.
Data availability statement: The datasets used and/or analyzed during the current study are available from the Global Burden of Disease (GBD) Data Exchange database (http://ghdx. healthdata.org/gbd-results-tool).
References
- World Health Organization. Mental Disorder 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-disorders. 2021.
- American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 2013.
- Conus P, Macneil C, McGorry PD. Public health significance of bipolar disorder: Implications for early intervention and prevention. Bipolar Disord. 2014; 16(5): 548-56. doi: 10.1111/bdi.12137
- Morselli PL, Elgie R, Cesana BM. GAMIAN-Europe/BEAM survey II: Cross-national analysis of unemployment, family history, treatment satisfaction and impact of the bipolar disorder on life style. Bipolar Disord. 2004; 6(6): 487-97. doi: 10.1111/j.1399-5618.2004.00160.x
- Bonnin CDM, Reinares M, Martinez-Aran A, et al. Improving Functioning, Quality of Life, and Well-being in Patients With Bipolar Disorder. The international journal of neuropsychopharmacology. 2019; 22(8): 467-77. doi: 10.1093/ijnp/pyz018
- Dols A, Thesing C, Wouters M, et al. Burden on caregivers of older patients with bipolar disorder. Aging Ment Health. 2018; 22(5): 686-91. doi: 10.1080/13607863.2017.1297360
- Mu L, Yu F, Xia J, et al. Association between high BMI and high homocysteine levels in Chinese patients with bipolar disorder. Journal of affective disorders. 2021; 295: 284-90. doi: 10.1016/j.jad.2021.08.032
- Azzini E, Ruggeri S, Polito A. Homocysteine: Its Possible Emerging Role in At-Risk Population Groups. International journal of molecular sciences. 2020; 21(4). doi: ARTN 142110.3390/ijms21041421
- Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. The Lancet Psychiatry. 2016; 3(2): 171-78. doi: 10.1016/s2215-0366(15)00505-2
- Ferrari AJ, Santomauro DF, Herrera AMM, et al. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. The lancet Psychiatry. 2022; 9(2): 137-50. doi: 10.1016/S2215-0366(21)00395-3
- He HR, Hu CY, Ren ZH, et al. Trends in the incidence and DALYs of bipolar disorder at global, regional, and national levels: Results from the global burden of Disease Study 2017. Journal of psychiatric research. 2020; 125: 96-105. doi: 10.1016/j.jpsychires.2020.03.015
- Zhang L, Cao XL, Wang SB, et al. The prevalence of bipolar disorder in China: A meta-analysis. Journal of affective disorders. 2017; 207: 413-21. doi: 10.1016/j.jad.2016.08.062
- Zhang YS, Rao WW, Zeng LN, et al. Prevalence and correlates of bipolar disorder in the adult population of Hebei province, China. Journal of affective disorders. 2020; 263: 129-33. doi: 10.1016/j.jad.2019.11.104
- Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. The lancet Psychiatry. 2019; 6(3): 211-24. doi: 10.1016/S2215-0366(18)30511-X.
- Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020; 396(10258): 1204-22. doi: 10.1016/s0140-6736(20)30925-9
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Cause List Mapped to ICD Codes Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME). 2021. http://ghdx.healthdata.org/record/ihme-data/gbd-2019-cause-icd-code-mappings
- Ou ZJ, Yu DF, Liang YH, et al. Analysis of the Global Burden of Disease study highlights the trends in death and disability-adjusted life years of leukemia from 1990 to 2017. Cancer Commun. 2020; 40(11): 598-610. doi: 10.1002/cac2.12094
- National Bureau of Statistics of China. Communiqué of the Seventh National Population Census (No.2). 2021. http://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817187.html
- Fellinger M, Waldhoer T, Konig D, et al. Seasonality in bipolar disorder: Effect of sex and age. Journal of affective disorders. 2019; 243: 322-26. doi: 10.1016/j.jad.2018.09.073
- Mayor S. Bipolar disorder: most patients receive suboptimal treatment, finds Scottish study. Bmj-Brit Med J. 2019; 364. doi: ARTN l95710.1136/bmj.l957
- Carvalho AF, Firth J, Vieta E. Bipolar Disorder. N Engl J Med. 2020; 383(1): 58-66. doi: 10.1056/NEJMra1906193
- Huang J, Yuan CM, Xu XR, et al. The relationship between lifestyle factors and clinical symptoms of bipolar disorder patients in a Chinese population. Psychiatry Res. 2018; 266: 97-102. doi: 10.1016/j.psychres.2018.04.059
- Marangoni C, Faedda GL, Baldessarini RJ. Clinical and Environmental Risk Factors for Bipolar Disorder: Review of Prospective Studies. Harv Rev Psychiatry. 2018; 26(1): 1-7. doi: 10.1097/HRP.0000000000000161
- Zhang X, Zhao M, Li J, et al. Associations between family cohesion, adaptability, and functioning of patients with bipolar disorder with clinical syndromes in Hebei, China. The Journal of international medical research. 2019; 47(12): 6004-15. doi: 10.1177/0300060519877030
- Wang Y, Yin J, Wang G, et al. Responsibility and Sustainability in Brain Science, Technology, and Neuroethics in China-a Culture-Oriented Perspective. Neuron. 2019; 101(3): 375-79. doi: 10.1016/j.neuron.2019.01.023
- Miller JN, Black DW. Bipolar Disorder and Suicide: a Review. Curr Psychiatry Rep. 2020; 22(2): 6. doi: 10.1007/s11920-020-1130-0.